Treatment of Keratoconus – Things You Should Know
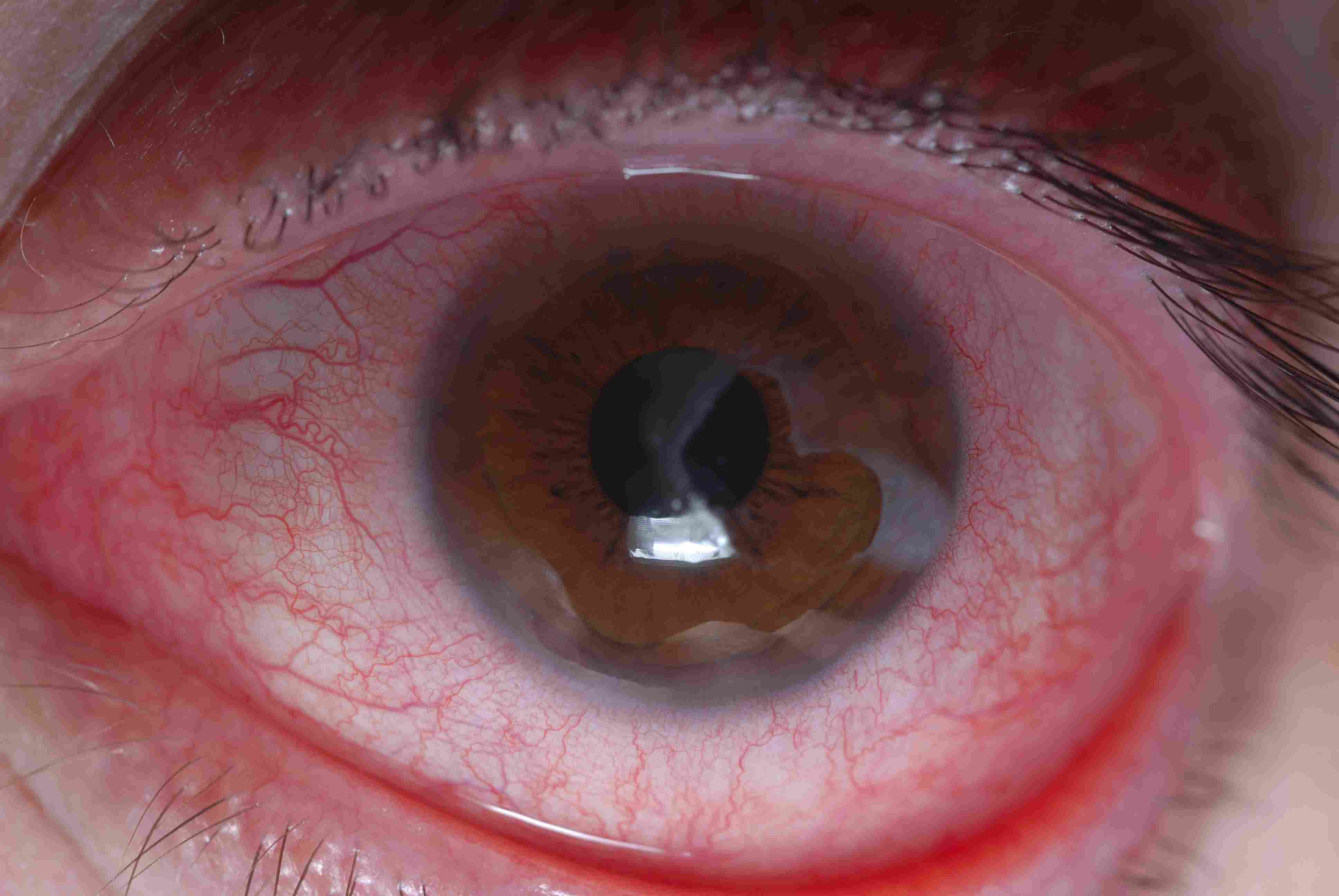
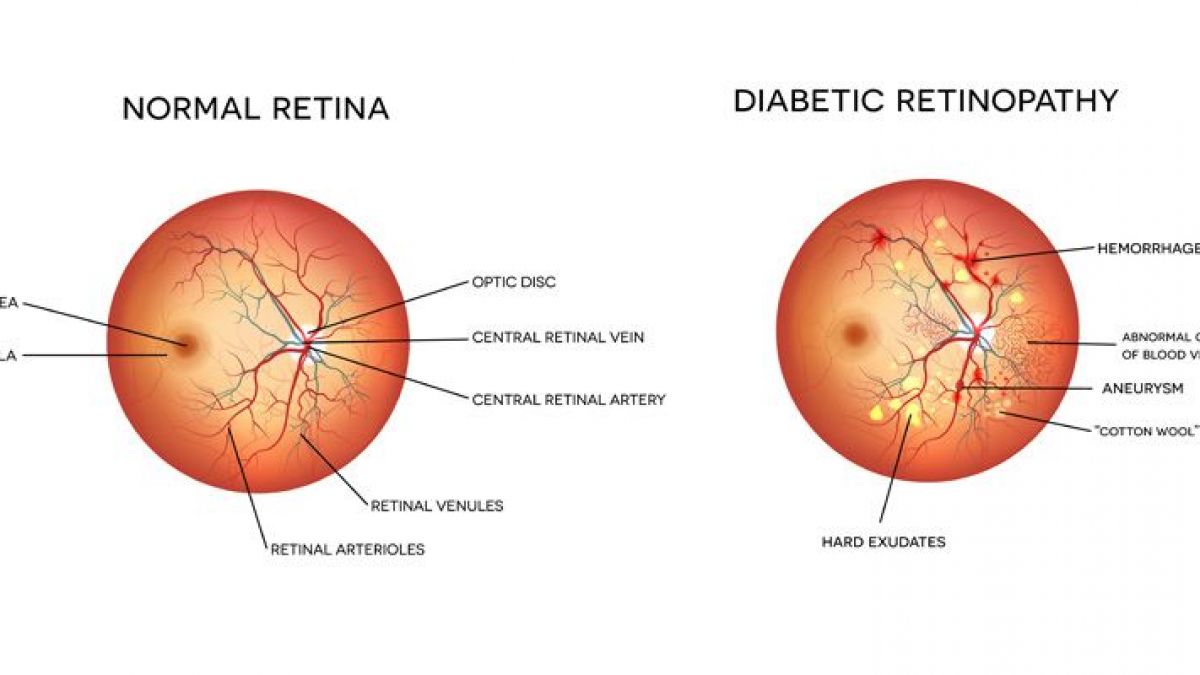
Keratoconus is a non-inflammatory, progressive, degenerative disorder characterised by thinning of the cornea – central or paracentral cornea starts to bulge and become cone-shaped instead. This process of thinning and re-shaping is termed corneal ectasia. This can make your vision distorted and blurry, as light being focused by your cornea forms an imprecise image on your retina, at the bac